Have you ever experienced the types of low back pain that surprise you while sleeping, laughing, or even just rolling around in bed?
Have you ever thought… "I must be getting older."
"Now I get hurt in my sleep!"
Yes, many people know back pain very well. If you have not experienced back pain, consider yourself lucky.
You will know when it happens. An instant pull or feeling of tightness followed by an intense, dull ache and excruciating pain. In a split second, all movement becomes painful.
Trying to stand hurts. Sitting hurts.
Sleeping hurts. Breathing hurts.
Tying your shoes becomes nearly impossible. Anything that involves bending forward or backwards… hurts.
But how did this happen? You barely moved and now you can barely move!
The pain will gradually subside over days to weeks and the next flare up may not come for months or even years, but when it does, it typically takes longer to recover.
Table of contents
What is low back pain (LBP)?
Low back pain or 'LBP' is a condition that affects over half a billion people globally everyday. In many cases, people suffering from low back pain tend to experience recurring episodes throughout their lifetime, which may eventually lead to disability.
Low back pain can affect people of all ages and is associated with physically demanding jobs, sedentary jobs, lack of physical activity, and obesity.
My patients with a flare up of low back pain typically describe the only position of comfort as lying on their back, feet elevated on a couch, and remaining still. Eventually, the pain lowers and the muscles relax, allowing just enough movement to get to the Ibuprofen.
After multiple rounds of hot packs and trying to "walk it off", the pain slowly fades away within a week to a month.
Over time, your back feels better and you return to your typical routine.
A few months later, after a long day of activity like manual labor, a theme park, or parenting, you gently move in the wrong direction and your back instantly "goes out." You are reminded of that day when you felt that pain and, now, it has returned, with a vengeance!
In some cases, there was no memorable popping moment or mechanism of injury that you can recall.
You simply moved awkwardly and now it hurts to move in ANY direction.
Why your back "goes out": the types of low back pain
First, it is important to understand the different types of back pain.
If you experienced a recent injury or direct trauma, for example a car accident or a fall, you should see your doctor before beginning an exercise program. You may have an injury and it is important to allow healing and avoid further damage.
In terms of chronic back pain, intense back pain flare ups, or a slow and progressive onset of back pain, there are a few subcategories to understand:
- Sacroiliac (SI) Joint pain
- Radicular pain
- Referred back pain
- Axial back pain
Sacroiliac (SI) joint pain
The Sacroiliac Joint (SI Joint) is where the sacrum connects to the pelvis. There are two SI joints, one on each side of the sacrum, where they articulate with the pelvis.

The sacrum moves with all forms of bodily motion and can be the source of pain if the joints move too much, or not enough.
In some cases, one SI joint will move less than normal, causing excessive movement and pain in the other SI joint. Other common reasons for SI joint paint or dysfunction include:
- Pelvic instability from postpartum recovery
- Diastasis recti
- Prostate surgery
- Abdominal surgery
- Hernia repair
- Various other genitourinary surgical procedures
Additionally, falling onto your buttock can cause an injury to the SI joint, especially if you land more on one side than the other.
A simple question I frequently ask:
"Can you point to your pain?"
If the person points directly to one of two spots on the low back, frequently called the low back dimples or "venus dimples"–this is called a positive "Fortin Sign". This indicates sacroiliac dysfunction.
The traditional approach to treat sacroiliac pain is to improve the mobility of the SI joints, and to stabilize the pelvic ring by strengthening the abs, pelvic floor, diaphragm, and back muscles.
For more info on SI pain and exercises, check out the postpartum exercise routine on the Go ARENA app.
Radicular back pain
When a nerve is compressed, entrapped, or pinched, we refer to this as radicular back pain. When a patient tells me the pain travels up or down the legs, this is the condition again which I run further checks and analysis.
As the nerve exits the lumbar spine, it travels around the hips, through the pelvis, and around the legs. Nerves do not stretch–instead, they glide through their designated pathways.
In cases of radicular back pain, the muscles along these pathways become tight, and their mobility decreases as a result. This leads to what's known as nerve entrapment.
In some cases, the nerve can be "trapped" or impinged where it exits the lumbar spine at the nerve root. Irritation of the nerve root can lead to sharp shooting pain down the leg.
Conservative treatment for radicular back pain aims to remove the pressure on the nerve, whether at the lumbar spine or at a muscle, and improve the ability of the nerve to glide through the soft tissue.
Referred back pain
Referred back pain can be described as pain felt in the back that originates from another region of the body. Vital organs refer pain to regions of the body that may feel like general low back pain, however, the actual dysfunction is in the organ.
There are two main cavities in the trunk: the thoracic cavity and the abdominal cavity. Both of these sections contain organs that are connected to the rest of the body.
In these areas, some of the neural connections overlap. In these cases, the pain may originate from an organ, but feels like its originating in the lower back.
For example, if someone has pain originating from a kidney, they may feel a dull ache or even sharp pain. This might be felt near the higher portion of the lower back–almost into the lower ribs!
Typically, referred back pain is considered when the aggravating or alleviating factors are difficult to identify. If you feel the type of low back pain described here and cannot make it feel better or worse with movement, rest, stretching, hot/cold, or stress relief, then the pain may be originating from a source other than your back.
Axial back pain
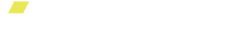
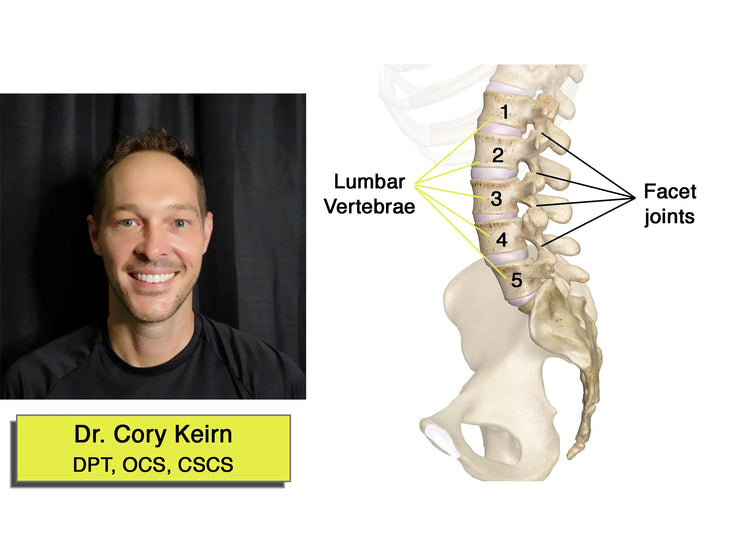
Axial back pain is very common, and flare ups of intense pain occur more often as you age! To explain managing it, we should first cover the anatomy of your lumbar region.
There are 5 lumbar vertebrae. Each vertebrae has 4 flat like joints (facet joints) that articulate, or move, with the vertebrae above and below.

When these joints do not move properly, it can lead to irritation, inflammation, pain with movement, and inevitably… low back pain.
Axial low back pain is usually the culprit when your back goes out from simply "moving the wrong way."
How routine motions contribute to low back pain
When we are young, we are able to move freely and with minimal pain. As we age, we fall into repetitive daily routines, whether it is our occupation, raising children, or performing daily duties.
This leads to us developing tightness in muscles frequently used and weakness in other muscles not frequently used. Over time, these muscular imbalances can lead to poor joint motion.
The lumbar vertebrae is like a ring with multiple muscle attachments in all directions. When muscles on one side of the ring become tight, they will pull harder on the vertebrae as it moves. This leads to poor joint motion and excessive friction on smooth joint surfaces.
Painful movement leads to guarded movement! This leads to stiff muscles and poor flexibility. Without guided movement and exercise, the muscular imbalances continue to progress as the stress on the lumbar spine increases.
Eventually, one wrong move and you feel like your back is stuck.
As the muscles relax, you may slowly regain your mobility. However, if you do not address the mechanical dysfunction, a flare up, or relapse, of the back pain may occur.
Our approach to treating lower back pain
If you're experiencing low back pain, we understand that your primary objective is to relieve this pain as quickly as possible! Here's how we typically recommend treating your low back pain symptoms in a simple and effective way.
Initially, the goal is to remove the stress on the lumbar spine and let it rest. This means keeping a neutral lumbar spine while bending, lifting, standing, and sitting.
As the pain subsides, the next goal is to gradually improve the spinal mobility within a pain free range. If you move too far into a painful motion, for example bending too far backwards, the body may feel pain again. This will cause it to go into "protection mode", thereby increasing muscle tension and bracing for another painful motion.
When the body feels pain, it will protect itself by avoiding painful movements. If you feel pain when the spine bends, your body will find compensatory movement in surrounding areas, like the hips or thoracic spine, in order to achieve the same goal.
This leads to faulty mechanics and poor posture.
How to improve and prevent low back pain
The road to low back pain recovery is at your doorstep! Here's what you can do.
Step 1: Wake up the diaphragm and improve circulation
The diaphragm is like a giant muscle plunger that compresses and distracts both the upper thoracic cavity and the lower abdominal cavity.
 The upward dog yoga pose stretches the diaphragm and may help to relieve lower back pain.
The upward dog yoga pose stretches the diaphragm and may help to relieve lower back pain.
Improving the strength of the diaphragm muscle will improve your breathing, which will in turn, help your muscles relax.
Step 2: Separate the lumbar spine from the pelvis and strengthen the abdominal stabilizers
Low back pain limits lumbar mobility and can lead to excessive mobility in the hips and pelvis. By improving motor control of the pelvis, the lumbar spine will learn to move independently.
For this, try pelvic tilts like those demonstrated below:
The abdominal stabilizers are the deep muscles along the abs that act as stabilizers between the front of the pelvis and the ribs.
Star side planks like those demonstrated below are wonderful abdominal stabilization exercises! Planks of any sort will do.
Step 3: Improve loaded spinal mobility
Your spine is designed to withstand forces from all directions. It is important to move your spine once the pain subsides and the irritation is removed.
The Standing T-Spine Windmill drill is a great exercise for this very purpose!
By gradually applying a light load with controlled movement, your body will become more confident and controlled in unstable positions!
Step 4: Improve trunk stability with dynamic movement
Lastly, you'll want to work on greater motion and flexibility in your trunk, where muscles may be tight and nerve endings may be entrenched. We recommend practicing rainbow leg lifts like those below to alleviate any lower back pain you may be experiencing.
Train your body to brace and stabilize when needed, but also to stay loose and relaxed. Take your time when approaching exercises designed to improve trunk stability to minimize your chances of re-aggravating any previous pain points!
To get the ARENA platform gym unit used to demonstrate these exercise, you can find their product page and checkout options here.
Resources:
- Cannata, F.; Vadalà, G.; Russo, F.; Papalia, R.; Napoli, N.; Pozzilli, P. Beneficial Effects of Physical Activity in Diabetic Patients. J. Funct. Morphol. Kinesiol. 2020, 5, 70. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.; Horton, R. Low Back Pain: A Major Global Challenge. Lancet 2018, 391, 2302. [Google Scholar] [CrossRef]
- Hartvigsen, J.; Hancock, M.J.; Kongsted, A.; Louw, Q.; Ferreira, M.L.; Genevay, S.; Hoy, D.; Karppinen, J.; Pransky, G.; Sieper, J.; et al. What Low Back Pain Is and Why We Need to Pay Attention. Lancet 2018, 391, 2356–2367. [Google Scholar] [CrossRef][Green Version
- Hoy, D.; Brooks, P.; Blyth, F.; Buchbinder, R. The Epidemiology of Low Back Pain. Best Pract. Res. Clin. Rheumatol. 2010, 24, 769–781. [Google Scholar] [CrossRef]
- Mattiuzzi, C.; Lippi, G.; Bovo, C. Current Epidemiology of Low Back Pain. J. Hosp. Manag. Health Policy 2020, 4, 15. [Google Scholar] [CrossRef]
- Papalia GF, Petrucci G, Russo F, Ambrosio L, Vadalà G, Iavicoli S, Papalia R, Denaro V. COVID-19 Pandemic Increases the Impact of Low Back Pain: A Systematic Review and Metanalysis. International Journal of Environmental Research and Public Health. 2022; 19(8):4599. https://doi.org/10.3390/ijerph19084599
- Ruffilli A, Neri S, Manzetti M, Barile F, Viroli G, Traversari M, Assirelli E, Vita F, Geraci G, Faldini C. Epigenetic Factors Related to Low Back Pain: A Systematic Review of the Current Literature. International Journal of Molecular Sciences. 2023; 24(3):1854. https://doi.org/10.3390/ijms24031854
- Russo, F.; Di Tecco, C.; Fontana, L.; Adamo, G.; Papale, A.; Denaro, V.; Iavicoli, S. Prevalence of Work Related Musculoskeletal Disorders in Italian Workers: Is There an Underestimation of the Related Occupational Risk Factors? BMC Musculoskelet. Disord. 2020, 21, 738. [Google Scholar] [CrossRef
- Shiri, R.; Falah-Hassani, K.; Heliövaara, M.; Solovieva, S.; Amiri, S.; Lallukka, T.; Burdorf, A.; Husgafvel-Pursiainen, K.; Viikari-Juntura, E. Risk Factors for Low Back Pain: A Population-Based Longitudinal Study. Arthritis Care Res. 2019, 71, 290–299. [Google Scholar] [CrossRef][Green Version
- Urits, I.; Burshtein, A.; Sharma, M.; Testa, L.; Gold, P.A.; Orhurhu, V.; Viswanath, O.; Jones, M.R.; Sidransky, M.A.; Spektor, B.; et al. Low Back Pain, a Comprehensive Review: Pathophysiology, Diagnosis, and Treatment. Curr. Pain Headache Rep. 2019, 23, 23. [Google Scholar] [CrossRef]
- Vadalà, G.; De Salvatore, S.; Ambrosio, L.; Russo, F.; Papalia, R.; Denaro, V. Robotic Spine Surgery and Augmented Reality Systems: A State of the Art. Neurospine 2020, 17, 88–100. [Google Scholar] [CrossRef][Green Version]